Beyond Medical Forms: Why Your Religious Identity Matters in Hospital Care
Religion
2025-03-27 18:28:18Content

My unexpected encounter in a bustling New York City emergency room caught me completely off guard. As I sat there, surrounded by the controlled chaos of medical professionals and anxious patients, a simple yet profound question was posed to me—one that initially left me speechless.
In that moment of vulnerability, I hesitated, unsure how to respond. The question hung in the air, laden with significance, while my mind raced to formulate an appropriate answer. Now, with the wisdom of hindsight, I realize the importance of being prepared and direct.
That experience taught me a valuable lesson: when faced with unexpected inquiries, especially in critical situations like a medical emergency, clarity and honesty are paramount. What once seemed like an intimidating moment has transformed into a powerful learning opportunity about communication and self-awareness.
Today, I approach such interactions with confidence, understanding that my response can make a meaningful difference. The ER encounter was more than just a medical visit—it was a pivotal moment of personal growth and understanding.
Navigating Personal Boundaries: A Patient's Guide to Medical Privacy in Emergency Settings
In the high-stress environment of emergency medical care, patients often find themselves confronted with challenging personal questions that test the boundaries of privacy and comfort. The intersection of medical necessity and individual autonomy creates a complex landscape where personal choices and professional protocols collide, demanding a nuanced understanding of patient rights and medical communication.Empowering Yourself in Vulnerable Medical Moments
The Unexpected Interrogation: Understanding Medical Intake Procedures
Emergency room intake processes are designed to gather critical information quickly, but they can sometimes feel invasive and overwhelming. Medical professionals are trained to collect comprehensive patient data, which may include sensitive personal details that patients might find uncomfortable sharing. The delicate balance between obtaining necessary medical information and respecting individual privacy creates a complex dynamic that requires careful navigation. Healthcare institutions have developed standardized intake protocols that aim to ensure comprehensive patient care. These procedures often involve a series of questions that might seem intrusive but are fundamentally rooted in providing the most effective medical treatment possible. Patients must understand that while they have the right to maintain personal boundaries, certain information can be crucial for accurate diagnosis and appropriate care.Psychological Dimensions of Medical Questioning
The psychological impact of unexpected personal questions during medical emergencies cannot be understated. Patients experiencing physical distress are simultaneously managing emotional vulnerability, which can make seemingly routine inquiries feel particularly challenging. Cultural backgrounds, personal experiences, and individual comfort levels significantly influence how individuals perceive and respond to medical interrogations. Psychological research suggests that patients who feel empowered and informed are more likely to engage constructively with healthcare providers. This empowerment comes from understanding the rationale behind specific questions and recognizing one's rights within medical settings. Communication strategies that prioritize patient dignity and consent can transform potentially uncomfortable interactions into collaborative healthcare experiences.Legal and Ethical Considerations of Patient Privacy
Medical privacy laws provide critical protections for patients, establishing clear guidelines about information collection and disclosure. The Health Insurance Portability and Accountability Act (HIPAA) in the United States, for instance, creates robust frameworks that balance medical necessity with individual privacy rights. These regulations ensure that patients maintain significant control over their personal information while allowing healthcare providers to deliver optimal care. Ethical medical practice demands a holistic approach that respects patient autonomy while maintaining professional standards. Healthcare providers are increasingly trained to approach sensitive questions with empathy, cultural sensitivity, and a clear explanation of why specific information is being requested. This approach transforms potential confrontations into collaborative dialogues that prioritize patient comfort and medical effectiveness.Strategies for Navigating Uncomfortable Medical Interactions
Developing personal strategies for managing unexpected medical questions requires a combination of self-awareness, communication skills, and understanding of healthcare protocols. Patients can prepare by reflecting on their personal boundaries, understanding their rights, and developing clear, respectful communication techniques for medical interactions. Effective communication involves asking clarifying questions, requesting explanations for specific inquiries, and expressing personal comfort levels directly and professionally. By approaching medical interactions with confidence and clarity, patients can create positive, collaborative relationships with healthcare providers that prioritize both medical necessity and personal dignity.The Broader Context of Patient-Provider Communication
The evolving landscape of medical communication reflects broader societal changes in understanding personal privacy, consent, and professional boundaries. Technological advancements, changing cultural norms, and increased awareness of individual rights are continuously reshaping how medical professionals interact with patients. Healthcare institutions are increasingly recognizing the importance of patient-centered care models that prioritize individual experiences and perspectives. This shift represents a fundamental transformation in medical communication, moving from traditional hierarchical interactions to more collaborative, respectful engagement strategies that honor patient autonomy and medical expertise simultaneously.RELATED NEWS
Religion

Faith in the Classroom: Kentucky Teacher Accused of Blending Religion with Public School Lessons
2025-03-13 16:24:35
Religion
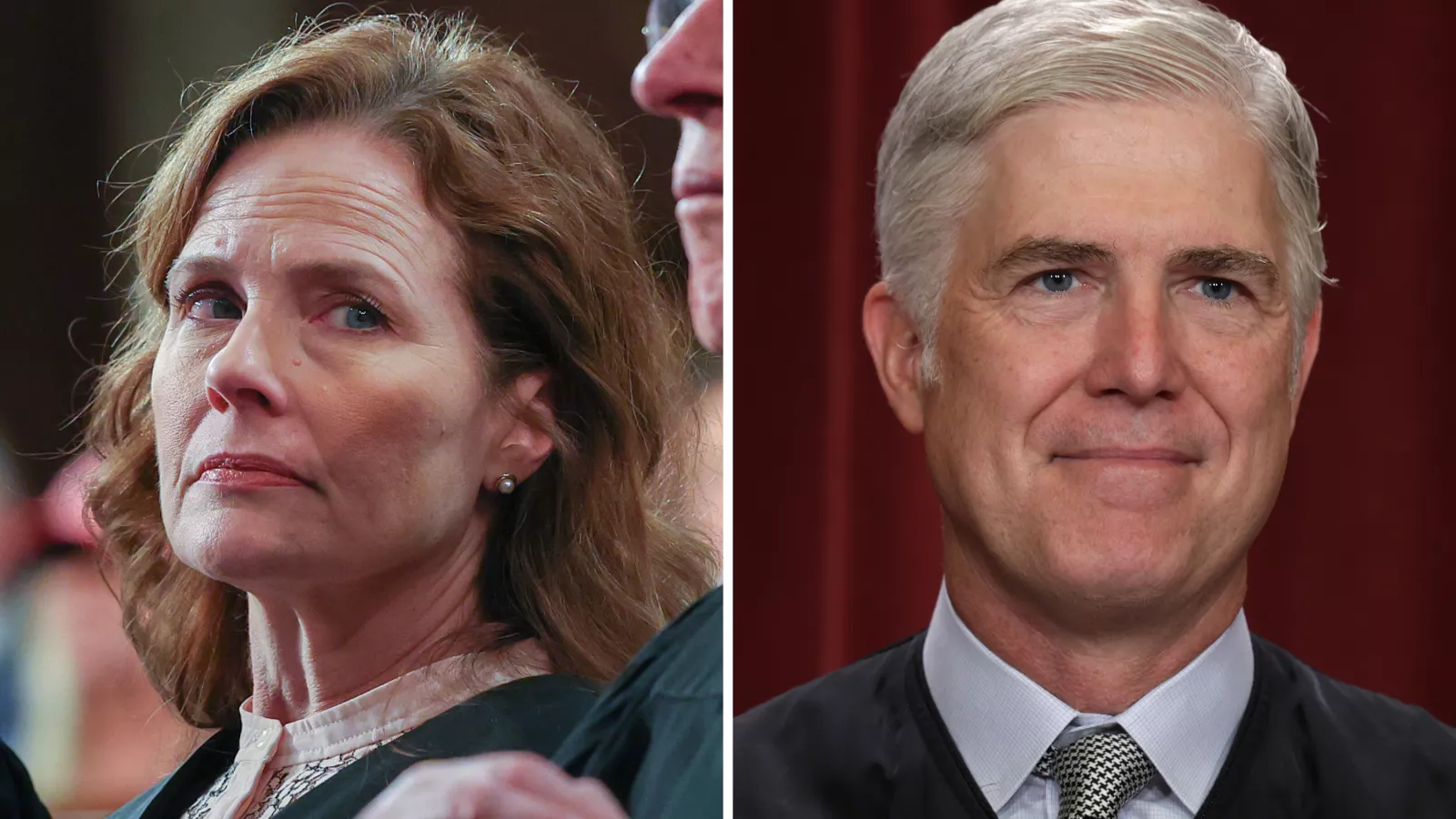
Supreme Court's Pivotal Moment: Justice Roberts Could Reshape Religious Education Landscape
2025-04-30 17:28:32